Haemoglobin
This lesson covers:
- How haemoglobin transports oxygen
- The factors affecting haemoglobin saturation
- The differences between fetal and adult haemoglobin
- The Bohr effect
- How carbon dioxide is transported by the bloodstream
How haemoglobin transports oxygen
Oxygen enters the lungs from atmospheric air and then needs to be transported to body cells.
Oxygen is transported to body cells via the blood:
- Red blood cells contain haemoglobin, which has haem groups.
- In the capillaries in the lungs, oxygen binds to iron in haem groups forming oxyhaemoglobin.
- Each haemoglobin molecule can carry four oxygen molecules.
- Oxyhaemoglobin can be transported via blood to respiring body tissues.
- At body cells, oxygen dissociates from haemoglobin.
Factors affecting haemoglobin saturation
Haemoglobin saturation with oxygen depends on the oxygen concentration, or partial pressure of oxygen (pO2). This can be shown on an oxygen dissociation curve.
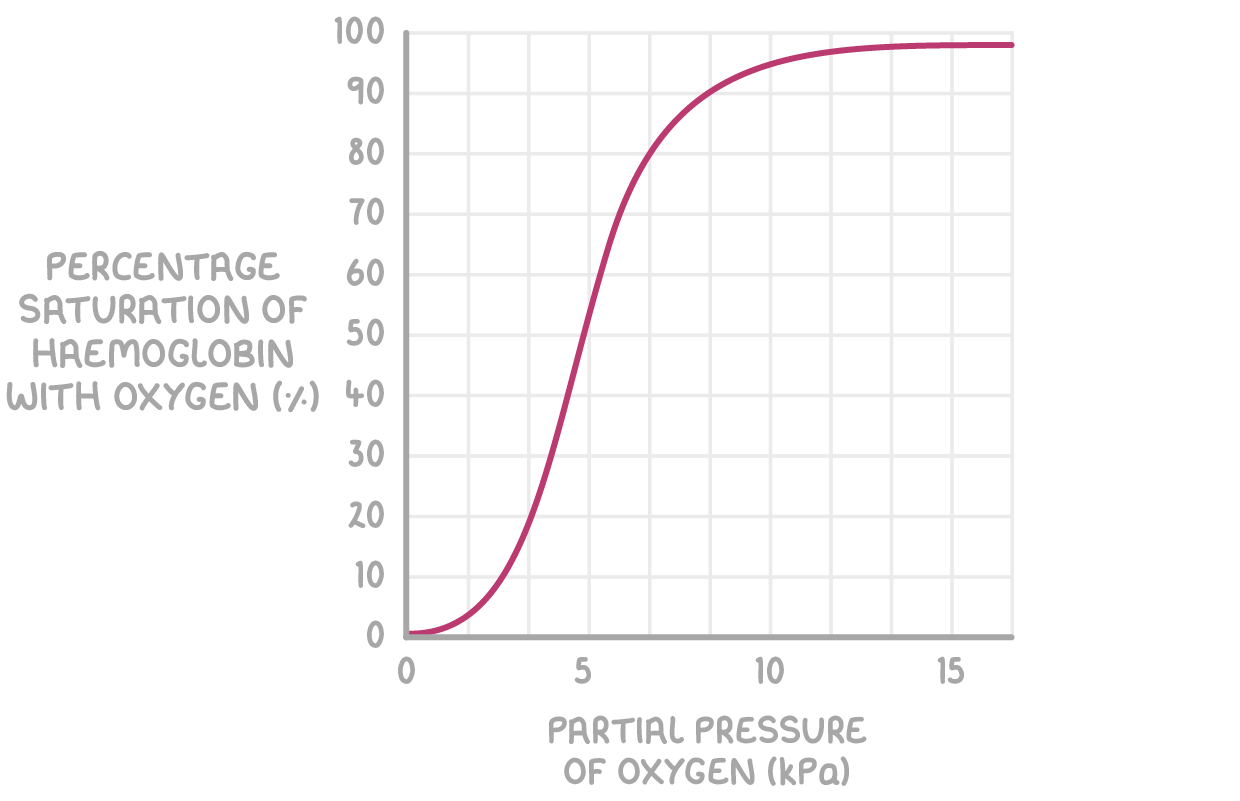
pO2 affects haemoglobin saturation as follows:
- Higher pO2 - Haemoglobin has a high affinity for oxygen and binds with it (e.g. in the lungs).
- Lower pO2 - Haemoglobin has a low affinity for oxygen and releases it (e.g. at respiring body cells).
The cooperative nature of oxygen binding
Haemoglobin saturation with oxygen also changes depending on how much oxygen has bound to it.
The cooperative nature of oxygen binding means that:
- When haemoglobin binds with one oxygen, it changes shape so it becomes easier to bind another oxygen.
- When haemoglobin is mostly saturated with oxygen, it is harder for more oxygen to bind.
Differences between fetal and adult haemoglobin
Fetal haemoglobin, which is the haemoglobin found in the red blood cells of an unborn fetus, differs from the haemoglobin found in a human adult.
Fetal haemoglobin differs from adult haemoglobin because:
- The fetus needs to obtain oxygen from the mother's blood.
- The fetal haemoglobin therefore has a higher oxygen affinity than the adult haemoglobin found in the mother's blood.
- This allows the oxygen to dissociate from the mother's haemoglobin, and bind with haemoglobin in the fetal blood.
- This ensures that the fetus gets enough oxygen to survive while it develops.
The Bohr effect
Haemoglobin also has a lower affinity for oxygen at higher partial pressures of carbon dioxide (pCO2).
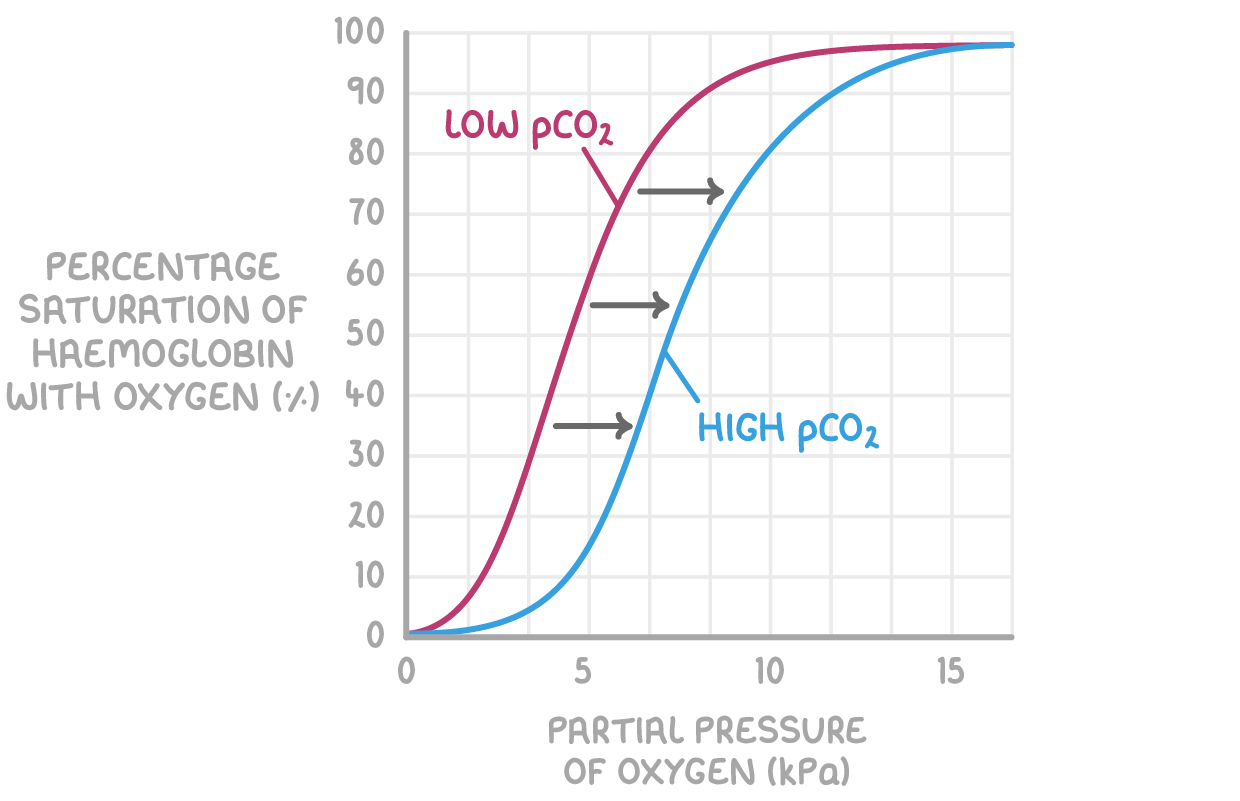
pCO2 affects haemoglobin saturation as follows:
- Higher pCO2 at respiring tissues causes haemoglobin to release oxygen.
- This is because of the Bohr effect, which is the decreased affinity for oxygen in haemoglobin when carbon dioxide is present.
- This means the oxygen saturation of haemoglobin is lower for a given pO2 when pCO2 is higher.
This is needed because the active tissues that produce carbon dioxide require a lot of oxygen from blood. The Bohr effect shifts the oxygen dissociation curve to the right, as seen by the blue line in the graph above.
Transport of carbon dioxide in the bloodstream
It is beneficial for CO2 to be converted into another form in the blood. This is because this maintains a steep diffusion gradient between respiring tissues, which need to get rid of CO2, and the blood, which removes this CO2 to the lungs.
There are multiple ways CO2 is transported via the blood:
- A small percentage of CO2 is transported dissolved in plasma.
- Some CO2 enters red blood cells, and is transported bound to haemoglobin as carbaminohaemoglobin.
- Most CO2 enters red blood cells and undergoes a reaction in the cytoplasm to form hydrogen carbonate ions.
The transport of carbon dioxide as hydrogen carbonate ions
Once CO2 from respiration enters red blood cells, it undergoes some changes in the cytoplasm so it can be transported as hydrogen carbonate ions (also called bicarbonate ions, or HCO3-). This process also explains why the Bohr effect occurs.
At respiring tissues, which have a high pCO2, the following occurs:
- CO2 reacts with water to form carbonic acid (H2CO3), catalysed by the enzyme carbonic anhydrase.
- H2CO3 dissociates to H+ and HCO3-.
- H+ binds to haemoglobin forming haemoglobinic acid, causing haemoglobin to release oxygen.
- This prevents the blood from becoming too acidic (H+ ions reduce pH).
- It also causes the Bohr effect: at high pCO2, haemoglobin releases oxygen so it can diffuse into respiring tissues.
- HCO3- ions leave red blood cells and are transported via plasma, while chloride ions (Cl-) enter red blood cells.
- This is called the chloride shift, and it maintains the charge balance by preventing excessive positive charge in red blood cells.
At the lungs, which have a low pCO2, the following occurs:
- The low pCO2 causes HCO3- and H+ to reform CO2.
- CO2 diffuses out of the body during expiration.