Types of immunity Immunity to a disease can be achieved in different ways: 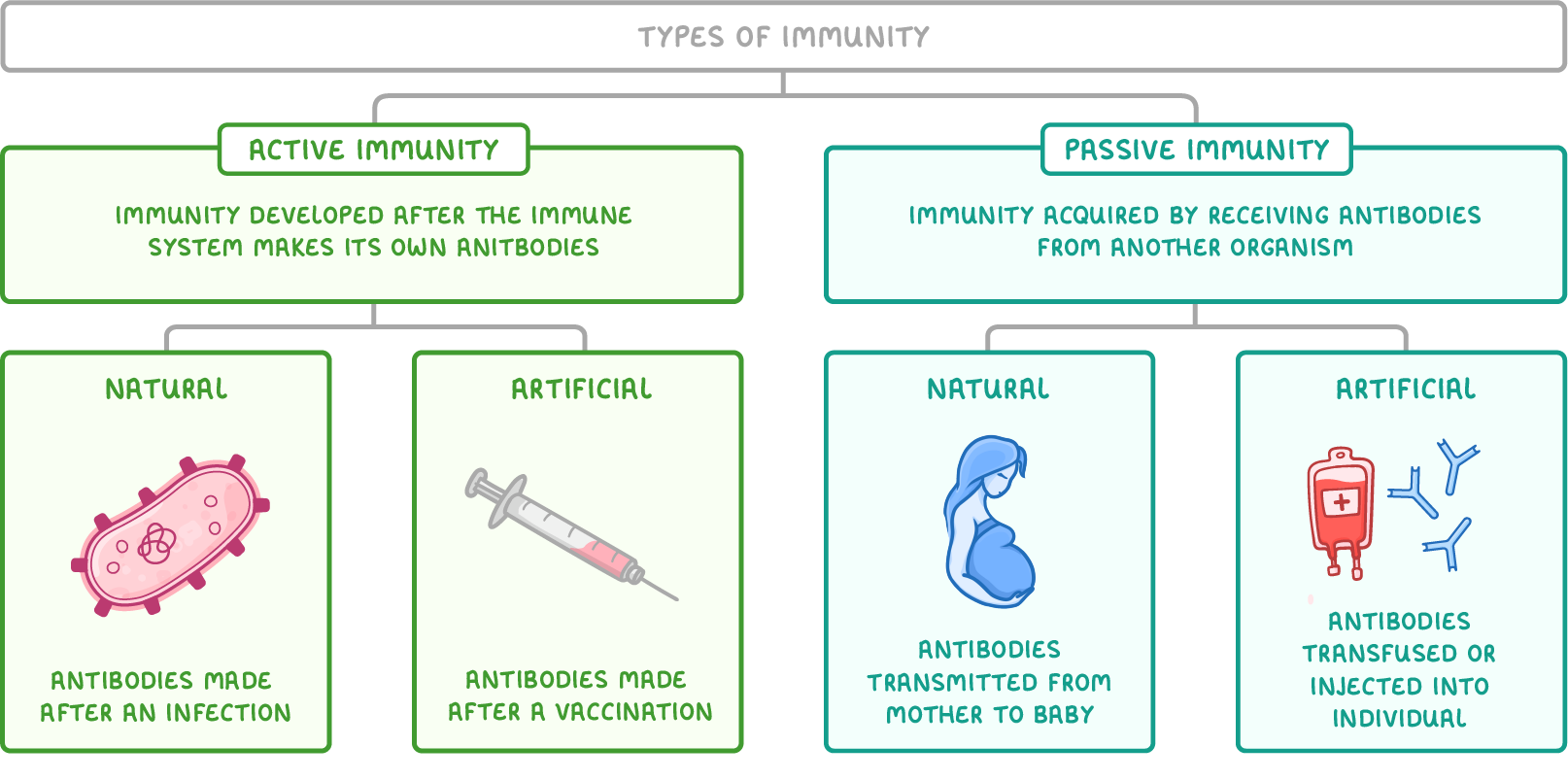 |
Active immunity:
Passive immunity:
|
Vaccination Vaccination involves the introduction of a pathogen's antigens into the body, usually via injection. This stimulates the body to produce an immune response to the pathogen and in doing so, allows the body to develop artificial active immunity. In order to produce an immune response, vaccines (the injected substance) usually contain antigens. However, they also need to be safe to prevent symptoms of the disease. Vaccines may contain any of the following:
|
How vaccination provides immunity Vaccination causes the body to produce antibodies against specific antigens. The main steps of vaccination are as follows:
Sometimes, booster vaccines need to be given later on to provide longer-lasting immunity. |
Criteria for a successful vaccination programme
When delivered well, vaccination programmes can prevent infection on a large scale.
However, there are a number of factors that affect how successful they will be:
- Availability - Suitable vaccines must be affordable and available in large amounts for mass immunisation.
- Minimal side effects - The fewer the side effects from the vaccine, the better the public acceptance.
- Infrastructure - Necessary resources for producing, storing, and transporting the vaccine are essential, including advanced technology and refrigeration.
- Administration - Proper and timely vaccine administration is important, requiring trained healthcare workers
- Herd immunity - The goal is to vaccinate the majority of the population to achieve herd immunity.
Herd immunity
Vaccines provide immunity to those that receive them, but they can also provide some protection to those not vaccinated. This is a concept known as herd immunity but it only works when a large proportion of a population are vaccinated.
Consider the two scenarios below.
Scenario 1
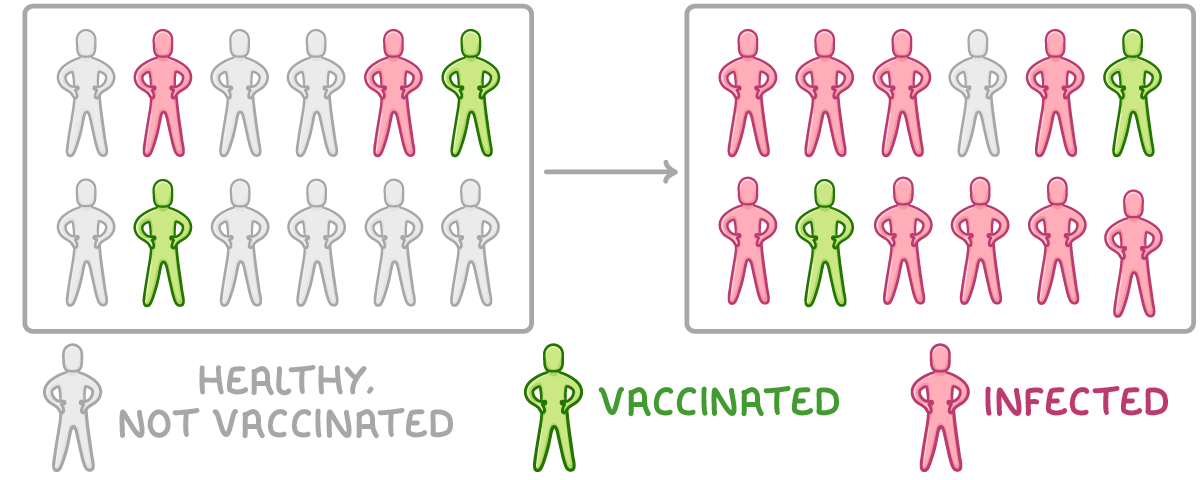
In this population, only a few individuals are vaccinated:
- This means that most of the population are susceptible to the disease, can be infected, and transmit the pathogen onto others.
- As a result, many individuals become infected.
Scenario 2
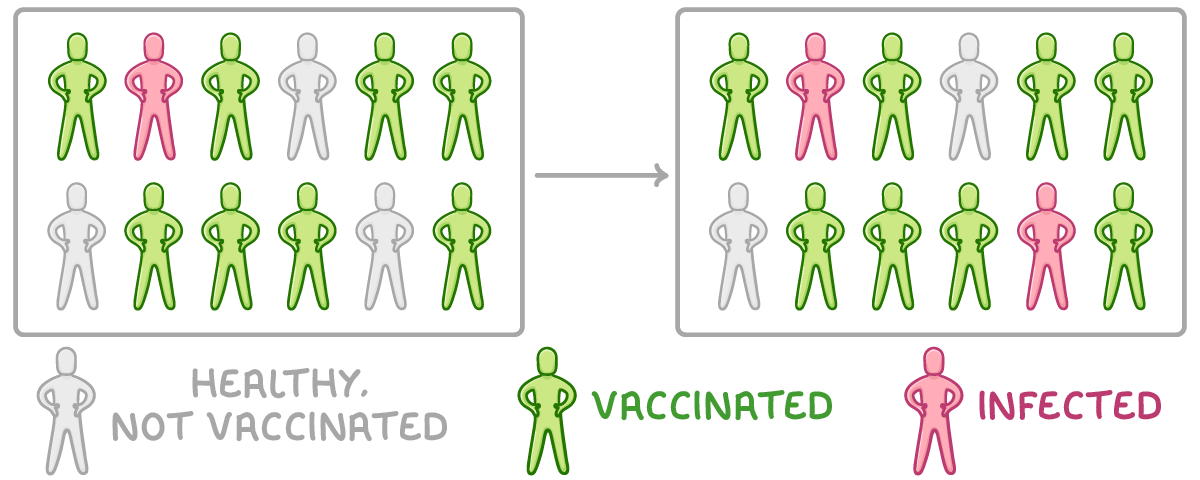
In this population, many individuals are vaccinated:
- This means that most people are immune to the disease and cannot transmit the pathogen onto others.
- This reduces the chance of non-vaccinated individuals coming into contact with the pathogen.
- As a result, fewer individuals become infected.
Mass vaccination of a population can help prevent epidemics and pandemics (the mass outbreak of disease). Herd immunity is important because it is never possible to vaccinate every individual within a large population (e.g. babies or individuals with compromised immune systems).
Why vaccines may not eliminate a disease
Despite meeting all the prerequisites for a successful vaccination programme, completely eliminating a disease can still pose a significant challenge.
Factors that may prevent the elimination of a disease:
- Individual immunity failures - People with weak immune systems (babies, elderly people, and patients with compromised immune systems) may not be able to withstand vaccines, or may not develop an immune response.
- Pre-immunity infection - Some individuals might contract the disease post-vaccination but before immunity develops, becoming potential disease reservoirs.
- Pathogen mutation and antigenic variability - Rapid antigenic changes due to frequent mutations can make vaccines ineffective, as the immune system can no longer recognise the pathogen's new antigens (e.g. with diseases like influenza).
- Pathogen variety - With diseases like the common cold, the sheer number of pathogen variants can make developing a universally effective vaccine nearly impossible.
- Pathogen hiding - Certain pathogens can evade the immune system by 'hiding' inside cells or inhabiting hard-to-reach body regions like the intestines (e.g. with cholera).
- Vaccine objections - Personal, religious, ethical, or medical objections to vaccination can hinder disease eradication. Misinformation can lead to reduced vaccination rates.
Antigenic variability
Vaccination relies on introducing a pathogen's antigens into the body to stimulate an immune response. However, some pathogens can change their antigens in a process known as antigenic variability.
Antigenic variability makes it difficult to develop vaccines against some pathogens because if the antigens change enough they will no longer be recognised by the immune system. This means that memory cells produced from vaccination against one strain will not recognise the antigens from another strain.
As a result, vaccines need to be changed frequently to provide protection against the most recent pathogenic strains.
Vaccination
This lesson covers:
- The differences between active, passive, natural and artificial immunity
- How vaccination works to protect against disease
- The concept of herd immunity